Falling Asleep vs Staying Asleep – Key Differences and Why they are Important
Problems involving sleeping can be summarized into a single sentence.“I can’t sleep.”“Of course, that applies only to doctors.” This is only the beginning for physicians.
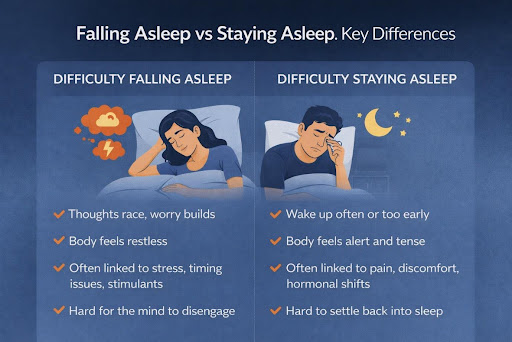
Therefore, not all sleeping difficulties are the same, even if the experience feels the same the next morning. Some people may have problems falling asleep in the first place. Some people may fall asleep easily in a short while but wake up throughout the night or much earlier than planned times. These two may sound alike, but not really when looking at them medically.
Knowing whether it is related to falling asleep or staying asleep can significantly change how physicians approach possible underlying causes, recommend lifestyle modifications, or consider possible courses of treatment. Both being considered as similar conditions often result in poor treatment strategies.
This is one of the key aspects of sleep health that is least appreciated or understood.
The Reason Why Physicians Break Sleep Disorders into Two Types
The two categories of sleep
There is not a simple on-off button when it comes to sleeping. It is an orchestrated process, and this occurs due to the various processes that function in the human brain and the human body.“When there is a problem with sleep, it is very useful to have information on where things start to go wrong,”Trouble sleeping tends to relate to issues in initiating sleeping, whereas trouble remaining asleep tends to relate to issues in sleeping maintenance. Neither share the same physiological mechanisms; both, however, cause fatigue.All this is why sleep medicine does not resort to universal advice.
What Trouble Falling Asleep Really Means
Difficulty falling asleep is described as the time it takes to fall asleep once one goes to bed. In medical terms, this occurs when an individual lies awake for a period of thirty minutes and even longer regularly.Individuals with this pattern have often described feeling tired yet unable to turn off. The body feels agitated. The mind feels busy. Ideas start racing. Minor concerns are magnified at night.
In terms of medical aspects, there is a very strong connection with arousal, but not with the pressure to sleep.
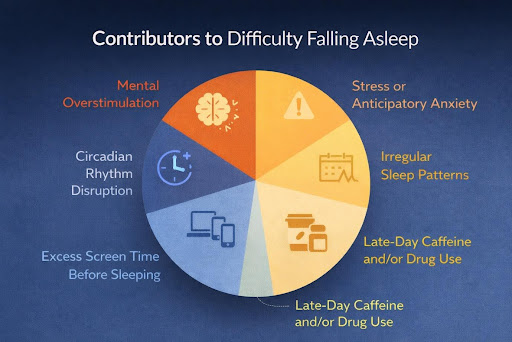
- Common Contributors Doctors Evaluate
- Mental overstimulation
- Stress or Anticipatory Anxiety
- Irregular sleep patterns
- Late-day caffeine and/or drug use
- Excess Screen Time Before Sleeping
- Circadian rhythm disruption
“The nervous system is on active alert when it should be slowing down. Physical exhaustion cannot overcome this condition readily.”
The Function of the Nervous System in the Onset of Sleep
Sleeping onset needs a transition from a state of alertness to a resting condition, which involves suppressing stress hormones and enhancing relaxation signals.When this transition does not happen seamlessly, the brain remains partially conscious. The body feels heavy; however, mental activity continues. The process of sleep becomes an effort rather than an automatic process.The pattern is quickly recognized by doctors because this condition will often resolve if the arousal levels are fixed instead of just increasing sleep times.
What Staying Up Might Look Like in Practice
Staying awake means awakening frequently throughout the night or waking up too early and being unable to fall back asleep.In contrast to problems with initiating sleep, these people tend to fall asleep easily. This problem emerges later, during a time when sleep should persist consistently.
This phenomenon is called clinical sleep maintenance insomnia.
Many people can describe waking up feeling alert. Many people also wake up feeling of being uncomfortable or experiencing pain or external stimuli. Their bed feels strange to them. Their body feels tight.
- Contributing Factors to Sleep Maintenance Issues in Patients with Sleep Disorders
- Chronic pain or physical discomfort
- Fluctuations inStress Hormones Peak During the Night
- Respiration disturbances
- Environmental sensitivity to noise or light
- Sleep Patterns
In most instances, wakefulness happens during the lighter phases of sleep, thus preventing the body from entering the restorative phases.
Why These Two Problems Feel So Different
Having trouble falling asleep is like a struggle in one’s mind. The mind resists sleep. Time passes slowly. A person experiences frustration.Trouble staying asleep is a more physical sensation. The body is what first wakes up. Awakeness comes suddenly. It’s as if a person could fall back asleep even though their mind is peaceful.This is important because it reveals that different systems are imbalance.
The Role of Sleep Patterns
Sleeping happens in cycles. Deep sleeping promotes physical healing. Light sleeping promotes memory and emotional control.Insomnia initiating sleep will not allow the entrance into the first cycle. Insomnia sleeping will not allow the continuation into the next cycles. In both scenarios, the net effect results in a decrease in the quality associated with sleep. However these patterns are examined by doctors because they impact how the body heals, handles pain, and copes with stress.
The Effects on Daily Activities
Both sleep issues affect one’s health but are usually presented differently.
Trouble sleeping often leads to mental tiredness, irritability, and problems concentrating. Trouble staying asleep often leads to physical fatigue, heightened pain sensitivity, and mood swings.
Usually, insomnia is found together with issues related to pain, inflammation, and hormonal changes. Difficulty initiating sleeping is commonly found together with issues related to stress and anxiety.
Why Generic Sleep Advice Often Fails
Many sleep guidelines are very general and not very helpful. A tip that helps one sleep pattern could very well ruin the other.For instance, intense sleep restriction could facilitate falling asleep faster but may increase nocturnal awakenings. Pain-related interventions can facilitate sleep maintenance but may not influence nocturnal restlessness.This is the reason why doctors stress the importance of diagnosis before recommendation or prescription.
How Doctors Assess Sleep Problems
Instead of depending on generalized information from patients, medical professionals have particularized queries. They ask how long it takes to fall asleep.“They also seek information on how often awakenings occur.”
In general, there seems to be a pattern.
- It enquires about sleeping times and regularities.
- They inquire about how the person feels during a day.
- These responses will direct further analysis and management.
- When Sleep Problems Become Chronic
- Short-term disruptions in sleep are very common. Special events or even illness may disturb sleep patterns.
If problems lasts for weeks and months, physicians investigate further. Underlying chronic disruption of sleep rarely occurs by itself and often co-exists with stress, pain, changes in mood states, and/or physical illnesses.In many cases, addressing sleep alone without considering these factors will result in an incomplete resolution of sleep disturbances.
The Relationship Between Pain and Sleep Maintenance
Pain and sleep are related in a bidirectional manner. Pain affects sleep. Lack of sleep leads to low pain tolerance.A common problem for those suffering from chronic pain is fragmented sleep patterns. Each time an individual wakes up, he or she will have an elevated level of sensitivity the next day, hence promoting the two conditions.Physicians understand this relationship and often treat sleep at the same time as they treat pain.
When Medical Guidance Is Must
When sleep problems interfere with daily functioning, concentration, mood, or physical recovery, it is very important to seek a professional evaluation.
Doctors can look at making changes in behavior, changes in sleep habits, cognitive-interventions, or following a treatment plan depending on the pattern identified. Sometimes, medication support may also be a topic of discussion if sleep and quality of life are being seriously influenced.
These issues are individualized and closely tracked.
- How Patients Can Help Explain Their Sleep Pattern
- Observe whether this struggle occurs prior to sleep and/or during the night.
- Record the time it takes to actually fall asleep.
- Notice when awakenings happen.
- Look out for pain or discomfort.
- Note your morning energy level.
- Detailed descriptions enhance medical decision-making.
Why the Distinction Makes All the Difference in Results
It can often go a long way to recognize if it is a problem of falling asleep or staying asleep. This helps doctors steer clear of trial and error and zero in on systems that are involved.This comprehension also lessens frustration. Understanding sleep disturbances can become less confusing when these disturbances are defined.
A Practical Next Step
When sleep disturbances continue even with simple modifications, an understanding of how sleep is assessed can help. The Sleep Wellness Guide discuss typical patterns and contributing factors for sleep and the role of healthcare providers in treatment decisions. The guides will not substitute for professional healthcare advice but are intended for the purpose specified above. Sleep is not just a matter of time spent in bed. It deals with movements within the state of rest. The difference between the onset of sleep and the maintenance of sleep is often where the improvement process should begin.
