Acute vs Chronic Pain – How Doctors Decide Treatment
Pain is one of the most frequent causes for visits to medical professionals but is also one of the most misconstrued. Two individuals may say they experience the same type of discomfort but will then receive two widely divergent courses of treatment for that discomfort. This is not inconsistent. This is classification.
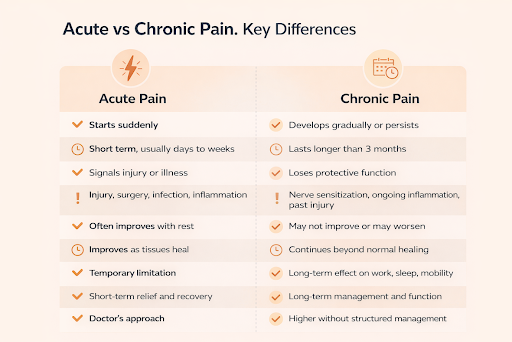
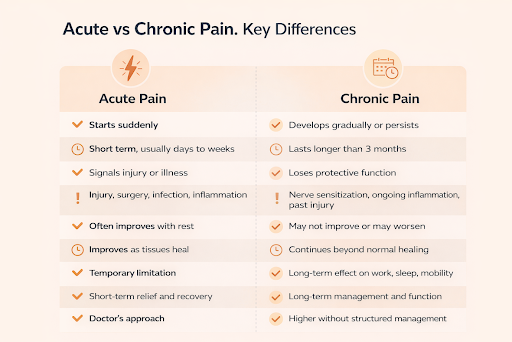
For a medical practitioner, pain conditions can fall into two broad categories, acute or chronic pain. The difference between the two impacts each and every decision, from the medical tests conducted to the actual medical treatment span, taken by a medical practitioner.
Why Pain Classification Matters
A physician does not treat an individual based upon how much he or she is suffering. How much an individual suffers and how long an individual has suffered create different conditions around which treatment must be based. Different pains respond differently when exposed to a different treatment modality. This is why healthcare professionals take the time to ask questions about the onset of the pain, its duration, and its change over time.
What is Acute Pain
Acute pain is usually short-lived and is related to the cause. It comes on suddenly and has a tangible onset.Examples include pain caused by injury, surgery, infection, or inflammation due to physical strain. Acute pain has a protective function. It informs the body of harm and promotes rest or avoidance while the body heals.In terms of clinical care, it can be assumed that the pain will get alleviated once the causing factor heals. In other words, the aim of treatment is managing the feeling of discomfort while the natural healing process takes place.
Most Common Features Found by Doctors:
Acute pain typically:
- Starts suddenly
- Has a clear trigger
- Improves over days or weeks
- Respects first-line treatments
Expectations are set for improvement, primarily for the easing of pain. Pain that fails to respond or improve within an expected time will give the physician reason to reconsider
How Acute Pain Is Treated
Treatment for acute pain is aimed at relieving and helping in recovery. Doctors are advised to follow a treatment plan involving rest and protection of the affected body part and over-the-counter medications for relieving pain.
In those patients where pain is intermediate in severity or impacts activity or sleep, medication assistance may be considered on a short-term basis. Even then, relief of symptoms is secondary to promotion of healing.
Follow up is necessary. The persistence of acute pain outside the expected period may indicate the onset of complications or the development of a new type of pain pattern.
What is Chronic Pain
Chronic pain is determined by its persistence and not intensity. It tends to go on for more than three months and persists after the normal healing time for the resulting tissue.
Acute pain differs from chronic pain because it usually preserves its protective role. Chronic pain becomes a state, while acute pain remains a symptom. Even after treatment of its cause, chronic pain can persist.Patients living with chronic pain often experience frustration. Resting does not relieve the pain. Simple treatments do not work. Pain becomes something that fits into the daily life instead of interrupting it.
How Chronic Pain Emerges
There are several ways in which chronic pain can occur. Inflammation, nerve sensitization, and alteration in central pain processing are some of them. With time, the nervous system changes. Pain tracts become more effective in relaying information. The brain becomes more aware of the discomfort. Pain sensitivity increases, even when there is minimal or no injury. The clinicians are aware of this phenomenon because of its impact on treatment goals.
How Doctors Assess Chronic Pain
When chronic pain is a problem, doctors start looking at things in a wider way. They no longer focus solely on what caused the original pain
Assessment will cover:
- Wording and description of symptoms
- Quality of sleep and fatigue
- Emotional Stress and Mental Health
- Functional limitations
- Prior response efforts and approaches
It aims to grasp in what manner pain impacts the individual, not in the location but as a whole.
Why Chronic Pain Demands a Different Treatment Approach
Chronic pain does not lend itself well to short-term solutions. Rest alone can actually increase stiffness and deconditioning. Short-term courses of treatment may offer symptom relief without actual improvement.They concentrate their efforts on the management of the pain and not so much on its removal altogether. This is not giving up; instead, it’s changing focus from cure to function and function to functionality and functionally stabilizing the life of the person. Treatment options might involve stratification and modification over time.
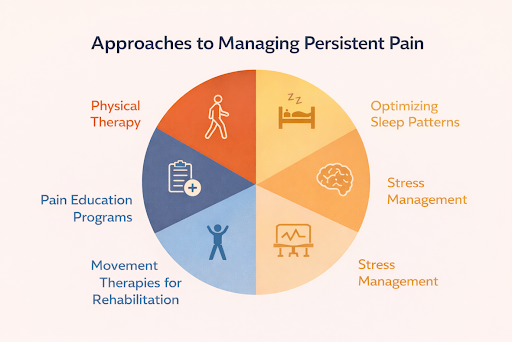
Treatment Approaches for Chronic Pain
Managing chronic pain usually involves a multimodal approach. The doctor might prescribe a number of methods based on the patient’s condition.These could include physical therapy, movement therapies for rehabilitation, optimizing sleep patterns, stress management, and pain education programs. In other instances, the use of prescription support services is recognized for the role they play in mitigating the severity of symptoms where pain has been impacting the patient’s ability to perform day-to-day functions. Decisions are personalized. One intervention doesn’t work for everyone.
How Doctors Decide Between Treatments.
The decision-making process is not easy. Doctors consider- Whether it be acute or chronic. Pain can be classified into
- How long symptoms have lasted
- Functional Impact on Work and Daily Activities
- Risk factors which increase susceptibility to a longer extent
- Patient preferences and concerns
This will enable patients to avoid unnecessary exposure to treatment while their pain will be taken seriously.
When Pain Becomes Irritable
Sometimes, pain can become irritable. Not all chronic pain begins in the chronic manner. Pain beginning acutely and persisting is common. Persistent acute pain becomes chronic. The doctor looks for symptoms like pain that persists even after expected healing times, heightened sensitivity, disrupted sleep patterns, and low activity levels. Early intervention helps to change the course of treatment accordingly. Early intervention helps avoid many long-term consequences.
What Patients Can Do to Ensure Better Outcomes
Pain patterns can be monitored to know if the pain is acting acutely or chronically. Information about sleep problems, activity restrictions, and stress symptoms is important. Open communication promotes safer and more effective treatment choices.
A Next Practical Step
If there has been more pain than expected or if it no longer responds to simple treatment like rest, knowledge of how doctors categorize pain can lead to taking additional steps. Pain Wellness Guide include explanations about pain patterns, the evaluation of pain, and various treatments that are easily understandable so that patients can discuss effectively with healthcare providers. Pain that persists needs serious consideration. The first discerning feature of pain management is determining if it is acute or chronic pain.
