What Makes Post-Surgery Pain Different than Normal Pain
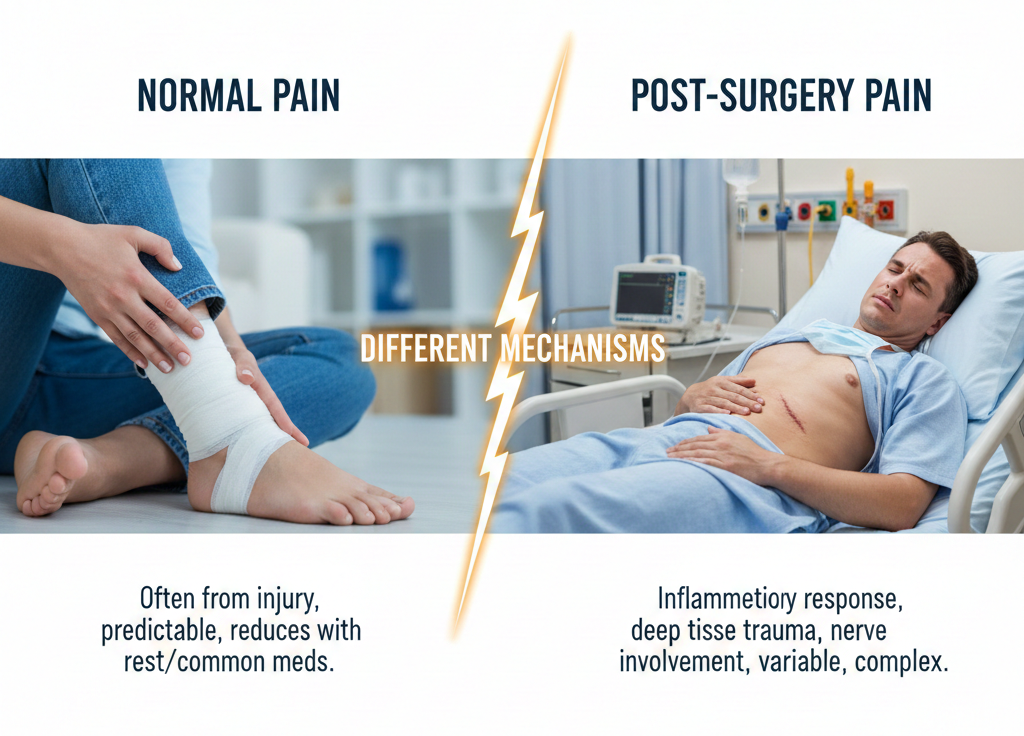
Pain after surgery is baffling. Individuals anticipate some degree of hurt and get ready to experience it, but they never know what the pain would be like. It is not as though it were an injury, or even muscle soreness, and it seldom progresses in a gradual, foreseeable manner.
The treatment of post-surgery pain varies as it is not only the damage pain that doctors deal with. Healing process, protective response of the body, and alterations in the nervous system all together give birth to it. The understanding of this assists the patients to heal easily and avoids panic upon the absence of a linear progression of pain.
Suffering in the after-readmission is a healing process
Once a surgery is done, the body enters a repair mode. The inflammation of the tissues is done intentionally, the blood circulation is accelerated, and the immune organs hurry to the location. The increase in pain signals is not an indication that something is wrong.
This discomfort causes the rest and constrained movement during healing. It is quite unlike excruciating pain that is the result of a continuing injury or illness.
The reason Pain Is Hard to Predict Post-Surgery
The stable daily improvement is an anticipation of many people, and in fact, the pain after surgery appears in waves:
One day feels better, the next feels worse, and even a trivial procedure may provoke the discomfort that appears to be disproportionate.
It does not necessarily imply that it is wrong. Tissues in the process of healing are delicate. Swelling may occur at different times. Perioperative nerves can be temporarily inconvenienced, and exhaustion can intensify pain. Physicians are concerned with trends, not a bad day.
The Nervous System Makes a Greater Impact than One Would think.
Surgery not only has an influence on the tissue, but the nervous system, as well. The brain is very alert on the affected part of the body, thus commands on the senses that are not rapidly felt are extreme. The effect of this increased sensitivity is protective initially. To others, the nervous system is slow to relax, thus the pain is present even during the healing period of the tissues. This is not a failure in surgery and it is only an indication that the nervous system is still getting used to it.
The Reason Why Movement Can Be Counterproductive and Beneficial at the same.
Post surgery movement is puzzling. Excessive movement is harmful; however excessively small movement is also damaging. Early mobilization helps in circulation, helps to eliminate stiffness and avoids complications. Nonetheless, premature and excessive movement may worsen pain. The protection and the gradual introduction of activity are the variables creating a balance, which vary every week among doctors. Suffering as a result of movement does not necessarily imply injury. Pain progressively worsening, or unreliably feeling better after rest, is to be taken notice of.
Post-surgery inflammation is to be anticipated
Postoperative inflammation is not remarkable. Normal healing involves swelling, warmth and tenderness and such inflammation may take a significant duration than the individuals anticipate, particularly after major operations. Inflammation usually aggravates at night. Fluid and circulation change throughout the day; resting with a lying position helps swelling to be relieved. Physicians anticipate this trend and assess it within the framework.
Scar Tissue and Change of Sensations
Scar tissue develops as the healing process takes place. Scar tissues do not act like normal tissue. It may become tight, achy in motion, and numb in certain professions and sensitive in others. These feelings are normal and they normally heal given time, however when sudden aggravation, burning up or extending pain occurs then it should be reconsidered.
When sleep can be affected by post-surgery pain
The cause of sleep disturbance is very prevalent in the post-operative period. Pain changes the position of sleep, lightens the sleep and maintains the alertness of the nervous system. Sleep deprivation at the time amplifies the pain sensitivity in the following days. When pain continues even post-surgery, doctors tend to inquire about the quality of the received sleep, as sleep improvement can also be used to suppress pain to a greater extent.
Stress Affects Recovery Pain in the Emotional aspect
Healing does not only involve the physical body. The factor of uncertainty, fear of re-injury, decreased progress speed, loss of independence, etc. are all elements that determine the way we experience pain. Stress causes the body of a person to tighten/ tone up, increases the activity of the nervous system and the pain to be experienced even when a normal healing is in process. The recognition of this linkage enables the patients to feel less scared of the changing symptoms.
Post-surgical Pain When it should be reviewed
It is natural that there will be pain in some cases; it is natural that some pain should be paid attention to. Concern in doctors occurs when post-surgical pain:
- Gets progressively worse rather than better on the whole.
- Companied with fever or contagious redness.
- Brings about new incentive or Heartlessness.
- Lives long after projected curing periods.
These indicators lead to additional assessment.
This is why it is unnecessary to enter into comparisons when it comes to recoveries.
Human beings tend to compare their recovery with other people. This causes unjustifiable anxiety. The recovery is based on: the operation, the affected tissue, the health before the operations, sensitivity to pain, stress and sleeping. Two individuals may undergo the same surgeries and considerably different recovery periods. Doctors do not care about comparison, it is progress that matters to them.
The Distinction between Pain Cure and Continued Pain
The process of healing pain alters slowly. It becomes less sharp. It becomes intermittent instead of constant. It is more responsive to motion and stillness. Persistent pain which fails to progress might require review. Physicians do not seek perfection but change.
The Reason Patience is an Addition to Treatment
The pain after surgery is better that way because improvement is not linear. The anticipation of a linear and quick recovery produces anxiety and this feeling makes people more sensitive to pain. Incoming information that fluctuations are normal makes the nervous system relaxed, which facilitates healing.
Patient Task and Activities in Recovery.
Patients may facilitate healing through:
- Adhering to movement instructions.
- Preventing the need to remain inactive.
- Protecting sleep routines
- Reporting changes clearly
- Avoiding self‑comparison
Effective communication assists doctors in making changes to care accordingly.
A Practical Takeaway
The pain after surgery is not same, since this is healing, sensitivity on the nervous system, and protection; it all occurs simultaneously. Discomfort does not necessarily imply harm, and pain does not necessarily imply a delay. Knowledge on what is normal will make the patients get back with confidence rather than fear.
Our Guides on Recovery after Surgery assist the patient in exploring and learning about the healing pattern and be ready to have a healthy conversation with their medical practitioner.
Healing is rarely silent. It communicates frequently with uneasiness before it calms down.
Pain Management Plans Expressed in a simple manner.
Management pain plans usually turn out to be more intricate that they are.
Physicians do not target pain plans to leave all the sensations; rather, they are aimed at returning to the work, enhancing sleep, and suffering in a safe way.
This knowledge causes pain care to seem less threatening and more cooperative.
The Actual Pain Management Plan.
A pain management plan is not treatment in one.
It is a methodology, which integrates:
- Assessing the type of pain
- Setting realistic goals
- Choosing appropriate tools
- Checking progress on a regular basis.
- The scheme varies with changing pain.
- The plan can be brief and specific in case of acute pain.
In case of continuous pain, it gets more extensive and adaptive.
The Why One-Size-Fits-All Strategy Is Not Working.
The way people appear on the surface can be different, yet in reality, pain is different.
Muscle pain, nerve pain, inflammatory and post-surgical exhibit different responses and treating them similarly would result in frustration.Physicians start by finding patterns: when the pain has begun, what exacerbates it, what helps, and how it impacts sleeping and life in general.
This basis influences the plan far much more than it is influenced by the intensity of the pain.
It is important to set the Right Goals.
One of the most significant sections of a pain plan is goal setting.
Doctors often focus on:
- Improving movement
- Supporting sleep
- Reducing flare frequency
- Increasing daily function
The first goal of pain elimination is not always realistic and safe. The movements of a progress are evaluated by the appearance of life and not only by the quality of pain. This change is useful in encouraging patients when the pain is not completely recovered.
Treatment includes Education.
An important component of the treatment consists of education.
Once the patients have the idea of how pain acts, they will not be anxious about each change, anxiety levels will reduce, muscles will relax, and the nervous system will become relaxed.
This is the only way the level of pain can be alleviated with time.
Pain education is not elitist; it is enabling.
Movement Is Not Left out.
Movement is a concept that is misjudged in pain care.
People are afraid of movements as it is painful, whereas doctors promote it, as not moving it tends to worsen the pain.
Typically pain management plans are:
- Gentle movement
- Gradual strengthening
- Activity pacing
It is not to put the pain through but to recondition the body to move safely once more.
Sleep Is a Core Focus
The relationship between sleep and pain is close. Sleep deprivation decreases the pain tolerance and persistent pain interferes with sleep.The physicians usually focus on sleep augmentation as an initial step. Improved sleep is beneficial in controlling pain, mood and curative ability.
When one neglects sleep, it becomes extremely difficult to handle pain.
The Stress and the Nervous System are discussed.
Pain is not just physical.
Stress also causes the nervous system to be awake, this intensifies pain.
Lesson plans that are developed to manage pain usually incorporate methods of decreasing the workload of the nervous system, like regular adjustments, relaxation exercises, or dealing with the worry over pain.
This does not mean that pain is entirely psychological but it appreciates the way the body decodes signals.
Drug Treatment Is a Part and not a Pharaoh.
A pain management plan may involve medication but it is hardly a plan as a whole.
Doctors consider:
- Short term use or long term use.
- Safety profile
- Communication with sleep and wakefulness.
- Effect on daily function
Decisions of medication are not final but reconsidered and changed.
Observation and Re-evaluation Should Be monitored.
A proper plan on pain involves follow up.
Doctors expect to reassess:
- What improved
- What did not
- Side effects
New symptoms
Whenever something is not helping, the plan is changed. This is not failure. It is responsible care.
The reason why pain plans change over time.
- Pain changes.
- Healing progresses.
- Stress levels shift.
- Activity levels increase.
What was a successful strategy in the early days might fail to succeed in the new times. Change is change and not failure.
Doctors seek trends and not perfection in everyday life.
What Patients might do to make Plans work better.
Treatment of pain can be effective when patients:
- Patterns of track, rather than bad days.
- Report effectively on changes.
- Movement guidance proceed slowly.
- Do not compare developments with others.
Clear feedback aids physicians to identify effective tailored care.
When a Pain Plan Needs Review
The following are some of the plans that should be reviewed:
- Instead of freezing up, pain aggravates.
- Sleep is becoming more and more despondent.
- New symptoms appear
- Function declines
- Treatment stops helping
These cues make reassessment and subsequent actions.
Why Simplicity Matters
Pain management must not be overwhelming.
The most effective plans are explicit, open and attainable. They are not dramatic solution oriented but gradual improvement oriented.
Plans need to be simple to follow. Less difficult plans are more effective in the long run.
A Practical Takeaway
Pain management plans do not constitute formulaic plans. They are considerate systems that are constructed around the person.
Treatment of pain as a process rather than a problem to eradicate results are better.
Our Pain Care Education Guide assist individuals to that of the plans and then engage evenly in their care.
Progress may be slow at times.
But with the right plan, it is rarely directionless.
